

Original article | Respirar, 2023; 15(3): 182-187 | ISSN 2953-3414 | https://doi.org/10.55720/respirar.15.3.4
Received:
July 3, 2023
Accepted:
August 18, 2023
José Manuel Araiza Sánchez
https://orcid.org/0009-0003-9574-7667
Juan José Espinoza Espinosa
https://orcid.org/0009-0004-4144-8407
Héctor Nova Félix
https://orcid.org/0009-0005-5290-1382
Eulalia Fernández Vallin
https://orcid.org/0009-0004-5902-5314
Esta revista está bajo una licencia de
Creative Commons Reconocimiento 4.0 Internacional.
Changes in Stress Index and Peak Inspiratory Pressure after Pneumoperitoneum in Laparoscopic Cholecystectomy
Cambios en el índice de stress y presión inspiratoria pico posterior a neumoperitoneo en colecistectomía laparoscópica
José Manuel Araiza Sánchez1 , Juan José Espinoza Espinosa1
, Juan José Espinoza Espinosa1 ,
,
Héctor Nova Félix1 , Eulalia Fernández Vallin2
, Eulalia Fernández Vallin2
1. Dr. Darío Fernández Fierro General Hospital, Anesthesiology, Mexico City, Mexico
2. Superior School of Medicine, National Polytechnic Institute, Department of Pharmacology, Mexico City, Mexico
Corresponding Author:
José Manuel Araiza Sánchez, manuelmangore@gmail.com
Abstract
Background: it is well known that pneumoperitoneum in laparoscopic surgery affects both cardiovascular and respiratory system, but it is not fully understood yet the degree in which we have to make changes in the ventilatory settings to minimize the complications due to insufflation of peritoneum, changes including impaired compliance and higher peak inspiratory pressures.
Methods: we collected data from 18 patients who underwent laparoscopic cholecystectomy and recorded changes in the airway peak inspiratory pressure and stress index before and after the beginning of pneumoperitoneum, starting at a Stress Index =1, then using Prism and SPSS, we ran the data through a T. Test for confidence intervals (CI) 95%.
Results: all 18 patients reported a significant shift in the airway pressures (p <0.005) and stress index when comparing them before and after pneumoperitoneum, with the same ventilatory settings.
Key words: stress index, peak inspiratory pressure, pneumoperitoneum, laparoscopic, protective ventilation.
Resumen
Introducción: es bien sabido que el neumoperitoneo en cirugía laparoscópica afecta tanto al sistema cardiovascular como al sistema respiratorio, pero no se entiende por completo el grado en el que debemos modificar los parámetros ventilatorios para minimizar las complicaciones debido a la insuflación del neumoperitoneo. Estos cambios incluyen disminución de la distensibilidad y mayores presiones inspiratorias pico.
Metodología: tomamos los datos de 18 pacientes que fueron sometidos a colecistectomía laparoscópica y documentamos los cambios en las presiones de la vía aérea e índice de stress (IS) antes y después del inicio del neumoperitoneo; iniciando con un IS = 1, posteriormente usando Prisma y SPSS, procesamos los datos a través de una Prueba T para un intervalo de confianza (IC) del 95%.
Resultados: los 18 pacientes reportaron un cambio significativo en la presión de la vía aérea (p<0.005) cuando se compararon antes y después del neumoperitoneo con los mismos parámetros ventilatorios al inicio de la anestesia.
Palabras clave: stress index, presión inspiratoria pico, neumoperitoneo, laparoscópica, ventilación protectora.
Introduction
A lung protective ventilation approach considers the use of a plateau pressure (Pplat) <25 mmHg and a tidal volume (Vt) of 6 ml/kg of the predicted body weight (PBW).1 However, these factors alone are not accurate enough to reduce ventilator-induced lung injury (VILI), and improve mortality in the patient under positive pressure ventilation (PPV). Driving pressure (DP), mechanical power (MP), and stress index (SI) have then appeared as surrogate markers of VILI more accurately associated with clinical outcomes.
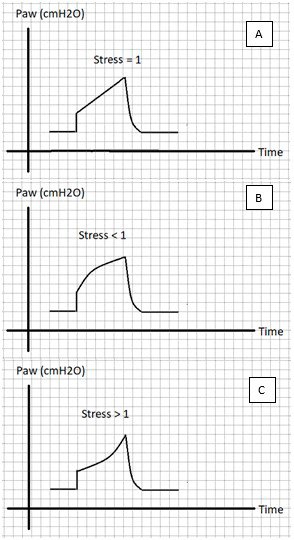
Stress Index can be assessed by analysing the airway pressure-time curve in the ventilator, translating the morphology of the curve into a number, either <1, 1, or >1, indicating alveolar collapse, adequate alveolar recruitment or overdistention, respectively (Figure 1). An adequate stress index can be associated with an improvement in lung dynamics, potentially reducing VILI in acute respiratory distress syndrome (ARDS) patients.1 Therefore, we could titrate PEEP and Vt to achieve a non-injurious ventilation with a SI = 1.2
During pneumoperitoneum in laparoscopic surgery, lung pressures are affected, and a decrease in lung compliance and an increase in chest wall resistance can be observed promoting alveolar collapse.3,4 We hypothesyzed that changes in Ppeak and SI could be observed after the onset of pneumoperitoneum, and that an adequation of ventilatory settings could potentially achieve a non-injurious ventilation.
Figure 1.
Representation of different Stress Index Paw curve morphology, where: A shows a SI = 1 as a straight ascending curve; B shows a SI < 1 as a descending upward concave curve; and C represents a SI > 1 as an ascending downward concavity curve.
Materials and methods
We performed a physiological study of patients undergoing elective laparoscopic cholecystectomy because the position during surgery tends to be less lung-injurious than other surgical procedures such as pelvic laparoscopic surgery and taking into account that Trendelemburg position doesn’t significantly affect lung dynamics during laparoscopic surgery.4 Inclusion criteria were: patients under general anaesthesia intubated, 18-60 years of age, scheduled for laparoscopic cholecystectomy, with previous written consent. Exclusion criteria were paediatric patients, and patients with previous lung disease (such as COPD, asthma, lung fibrosis).
Ethics were obtained from “Dr. Darío Fernández” General Hospital Research and Education committee in October 2022, and data was collected from November 2022 to February 2023.
Anaesthesia and ventilator management
Induction of general anaesthesia was performed with fentanyl at a dose of 4 mcg/kg, intravenous lidocaine 1 mg/kg, propofol 2 mg/kg and muscle relaxants used were cisatracurium besylate 0.1 mg/kg or rocuronium bromide 0.8 mg/kg depending on the patient’s characteristics or the anaesthesia attending criteria; there were no complications nor incidents in the intubation procedure in any of the studied patients.
Patients were connected to the Anaesthesia Machine (Drägger Fabius R Plus and Infinity R Empowered; Dräger Medical, Lübeck, Germany) and set to protective volume controlled ventilation parameters: Vt 6 mL/kg PBW, respiratory rate (RR) 16 – 18 rpm depending on the EtCO2 levels, I:E 1:2 – 2.5, inspiratory time >1 s, and PEEP to achieve a SI = 1 in the Pressure-time curve before the start of pneumoperitoneum.5-8
Sevoflurane was used for anaesthesia maintenance at a MAC 0.9 – 1.1. In all cases, all the patients were extubated after surgery with no reported complications or incidents and then delivered to the recovery room.
Statistical analysis
Stress index and Ppeak were measured before and after pneumoperitoneum. Data was analysed using Prisma Graphpad and SPSS (SPSS Inc., Chicago, IL), by s paired t Test. We estimated a sample size of 12 subjects by using a simple quantitative estimative sample size approach, A p value of 0.05 was considered as significant.
Results
We analyzed data from 18 patients, gender (female/male) 17/1 (94.4%/5.6%), age (y) 55 [25, 85]. One patient (5.6%) was a heavy smoker with a normal spirometry and was included in the study.
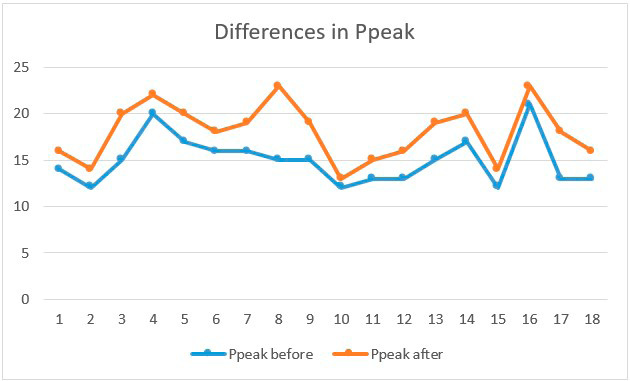
Stress index shifted from a baseline =1 to a <1 after the onset of pneumoperitoneum (p<0.05). Ppeak increased (14.9± 0.7 mmHg vs 18.1±1.41, p <0.005) mmHg. (Figure 2).
Figure 2.
Distribution of Ppeak (in mmHg) before (blue) and after (orange) in all the participants.
Discussion
Our main result was that during elective laparoscopic cholecystectomy, pneumoperitoneum induced a change in SI from 1 to <1 and an increase in Ppeak in all the patients. In this observational study, changes in stress index showed a tendency to alveolar collapse after the onset of pneumoperitoneum. Ventilator settings were adjusted to achieve a SI = 1 at baseline and changed to a value of <1 in all cases, even with a pneumoperitoneum of 12 cmH2O. Ppeak showed significant changes before and after pneumoperitoneum with the same Vt.
These results were consistent with previous reported studies, for example, Seoung et al. reported a significant change in dynamic compliance and peak inspiratory pressure after pneumoperitoneum, not affected by Trendelemburg position.4 Similar results concerning peak inspiratory pressure changes after pneumoperitoneum were reported by Hemmerling et al.13
Very few surrogate markers associated with ventilator-induced lung injury have demonstrated an impact on clinical outcomes. Stress index appears as a surrogate marker of potentially harmful ventilation, easily accessible by analysing the respiratory mechanics waveforms in the ventilator. 1,9
By analysing respiratory mechanics, particularly pressure-time curves during volume controlled ventilation, SI can be evaluated and adjusted to achieve a linear slope of the ascending limb of the pressure – time slope.10
Pneumoperitoneum has demonstrated to cause lung collapse, atelectasis, derecruitment and decreasing lung compliance; therefore, leading to the need of higher PEEP values in order to diminish its deleterious effects on lung dynamics.3 Therefore, a dynamic parameter such as SI, which represents the recruitment/collapse in the alveoli, would be affected by the high abdominal pressure caused by pneumoperitoneum.
Laparoscopic surgery has many advantages for the surgeon and patient, as a shorter recovery period and a lower risk of infections; however, ventilator management during pneumoperitoneum is a real challenge to the anaesthesiologist due to changes in lung dynamics, diaphragm impaired dynamics and circulatory changes.11 Ventilatory goals are directed to reduce VILI, improve ventilatory dynamics, improve early recovery after laparoscopic surgery.12
Limitations of this study included choosing the right time to register SI and Ppeak value due to surgeon manipulation in the surgical field. Therefore, we sometimes asked the surgeon to pause the procedure so we could take our data and then continue with the operation.
Conclusion
After evaluating changes in pulmonary pressures and stress index, we demonstrated a tendency to alveolar collapse and higher peak inspiratory pressure after pneumoperitoneum. Therefore, and although more studies are needed to verify these findings and potential implications, adjusting ventilatory settings during laparoscopic surgery in order to improve respiratory dynamics, and to achieve an adequate Stress Index associated with an adequate alveolar recruitment, and thus minimizing the incidence of ventilator-induced lung injury, could be of potential benefit to these patients.
Funding: none.
Conflict of interest: the authors declare no conflicts of interest.
Author’s contributions: JMAZ: project management, formal analysis, conceptualization, writing, review and editing, research, methodology, original draft. HNF: conceptualization, review, supervision, validation. JJEE: data curation, formal analysis, writing, supervision, validation. EFV: data curation, formal analysis, writing, supervision, validation.
The Editor in Chief, Dr. Carlos Luna, followed the review process and accepted this article.
References